Table of Contents
How’s Your Pain How’s Your Pain How’s Your Pain How’s Your Pain?
To purge onward with developing some semblance of chronic pain mastery (ha), my employer had the pleasure of hosting a mentor and good friend Adriaan Louw.
I first heard Adriaan speak in 2010 when I was in PT school. I was amazed at his speaking prowess and the subject matter. Unfortunately, my class could only stay for a little while in his course, and onward life went.
I went on with my career focusing on structure and biomechanics and forgetting about pain. It wasn’t until I ran into Adriaan again two years later. He was teaching me Explain Pain (EP), and forever changed how I approached patient care.
It’s funny how things have come full circle. Here we are, Adriaan teaching Therapeutic Neuroscience Education (TNE) through The International Spine and Pain Institute (ISPI), and me promoting his work to my colleagues.
A lot has changed in two years. EP and TNE are quite different courses, and I learned so much this weekend that I continue to become more engrossed with what I do.
So thank you, Adriaan, for playing a huge role shaping me into who I am today. I have now become very much more interested in what ISPI has to offer, and I think you should too. And no worries Adriaan, I will stay hungry 🙂
So without further ado, here is what I learned.
The Power of Words
It’s getting worse. One person out of 3.5 has chronic pain. Many of these people have tried many treatments, heard many explanations, and lost all hope.
And here they are, in your office. The patient thinks you are going to be another statistic. Another failure. Another person who can’t help them.
So what do you do?
The answer: Apologize, and tell them they are going to be okay.
These are some of the most powerful words in medicine, and likely words that these people with chronic pain have never heard. Most importantly, they satisfy the ultimate goal of TNE:
Reduce the perception of threat
That, my friends, is what all physical therapy interventions do. Exercise, manual therapy, and education all reduce threat perception. These simple words can often jump start the process.
Changing Cognition
Fear and catastrophization are often the big components that we have to battle with the above patients. When these beliefs regarding pain are present, a cycle of avoidance and disuse occurs. These factors can continually perpetuate the pain cycle.
When experiencing pain, we can go one of two routes.
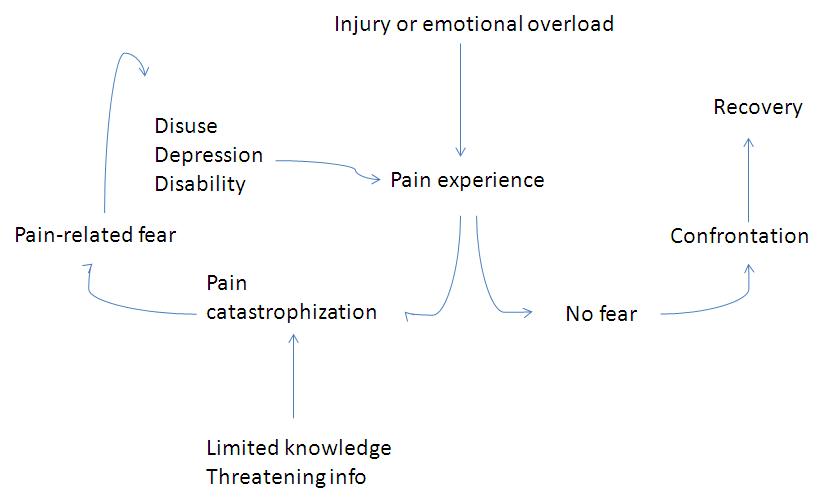
We can see how understanding pain can have profound impacts regarding recovery, yet the converse can lead to a debilitating cycle. Our goal is to steer people towards confronting their experience as quickly as possible. Knowledge can be powerful at reducing chronic pain.
Realize that there are many other factors that go into which path one will travel. These factors may include pain beliefs, sleep, behaviors, family, social circle, job, etc. These examples are a few of many variables that make pain as complex as it is.
The best that can be done is to manage the threats you are able to influence and educate the patient on understanding other possible factors.
Psychologist Wannabe
Now some of you psychology fans might be thinking that this strategy may be stepping into areas outside of our scope. But think of how we treat impairments that may be impacting one’s movement:
- Stiff joints – manual therapy
- Altered muscle recruitment – motor control
- Muscle stiffness –manual therapy
What if the impairment impacting one’s movement is one’s thoughts and beliefs? What intervention would you utilize to address this area?
Clockwise ultrasound of course.
The logical choice of course, would be educating the patient that these thoughts and beliefs do not relate to the pain experience. Successful education may affect the impairment shackling that person.
Educate
Why is it that when patients come to us in pain we teach them anatomy? This was a question Adriaan posed to the class that summed up my frustration with much of traditional orthopedics in a way I never could.
There are a few studies (here and here) that have demonstrated that educating patients on anatomy and biomechanics has limited efficacy and may increase fear. Moreover, using degenerative terms are associated with poorer prognosis (here).
The problem with this strategy is that it does not adequately address what the patient is seeing you for–pain. Fortunately, the evidence for TNE is becoming quite compelling (check it).
It’s All in the Delivery
So TNE sounds all well and good, but the question must be posited: how? There are several ways to skin this cat (as long as the cat gets skinned):
- Research demonstrates only performed by PTs currently.
- Sessions can last from 30 minutes to 4 hours, but Adriaan suggested 10-minute increments.
- 1on1 is best, but groups of 8-10 people are also good.
- Use props – pictures, drawings, metaphors, etc.
The research also demonstrates that certain content must be covered:
- Pain neurophysiology.
- No reference to anatomical or patho-anatomical models.
- No discussion of emotional or behavioral aspects to pain.
- Nociception and nociceptive pathways.
- Neurons.
- Synapses.
- Action potentials.
- Spinal inhibition/facilitation.
- Peripheral sensitization.
- Central sensitization.
- Plasticity of the nervous system.
One phenomenal way to gauge if patients understand your education is by having them fill out the Pain Neurophysiology Questionnaire (PNQ). This tool covers a large portion of TNE, and can give you talking points on where your education ought to be targeted.
I have been having patients fill this out for a few weeks now, and it is amazing how many people have pain misconceptions even after I perform TNE. Most of the learning that was occurring was superficial. This tool gives you reason to reinforce your education, as well as a way to have evidence of learning.
Now I have been talking a lot about education, and the common misconception is that all you do is talk to your patients. This thought is far from true. Most of the study designs in Adriaan’s systematic review had other interventions along with education. So it is only one piece of the puzzle. You do not have to completely change how you treat patients, you must only change the framework at which you educate and think.
Pain Neuroscience…Learn It!!
If you are going to explain pain to patients, you have to know more about it then they do. To enhance our knowledge base, we can discuss the PNQ in detail. So fill it out before reading on.
Go ahead, I’ll wait.
Did you fill it out yet?
Okay, here we go:
Pain receptors convey the pain message to your brain: FALSE
Why – Tissues only send danger messages. Compare suffering an ankle sprain on a sidewalk versus a busy street. The latter would not necessarily hurt.
Fun fact – There are no unmyelinated nerves in the body. Every axon wears a coat; it just depends on what degree
Pain only occurs when you are injured: FALSE
Why – Injury and pain are not synonymous. Think about when you get a bruise and are not aware of it.
Fun fact – Tissues heal in 3-6 months. This includes your bulging discs.
The timing and intensity of pain matches the timing and number of signals in danger messages: FALSE
Why – This statement predominately deals with descending modulation and interneurons. In acute pains that end quickly, danger messages make their way up to the spinal cord and then the brain, but the brain sends endogenous opioids down the system to turn the dial down on danger messages.
There are many other fibers that that send messages to the brain, one example being A-betas. These sensors carry information regarding light touch for example. If you occasionally feel that you are wearing pants (unless you are not), you can thank these fibers.
However, you don’t have to constantly be reminded that you are wearing pants, so an interneuron in the spinal cord will prevent this information from reaching the brain. The interneuron is like a club bouncer; only the VIPs pass.
However, if danger messages (via A-delta and C-fibers) continue firing to the spinal cord, the interneuron could potentially die from amino acid overload. When this change occurs, the club called your spinal cord has no bouncer, thus all information from the periphery will make it to the brain. This input barrage can significantly impact your body’s ability to modulate danger messages, and eventually pain.
Fortunately, interneuronal death takes months to years in most cases except when someone gets struck by lightning, electrically shocked, or in whiplash. But the message is clear; we must do what we can to modulate nociception and pain so this change does not occur.
The best way to treat chronic pain is to prevent it.
Nerves have to connect to a body part in order for that part to be in pain: FALSE
Why – Phantom limb pain, duh! The somatosensory homunculus is what allows for this phenomenon to occur.
When areas are used less, such as in pain states, the area of that body part becomes less clear. These changes can occur as fast as 30 minutes. The research shows the more “smudging” of these areas you have, the more pain you have.
So in phantom limb pain, the body part is gone, but the brain representation of that area remains.
In chronic pain, the central nervous system becomes more sensitive to danger messages from tissues: TRUE
Why – Interneuron death plays a role, but also descending influences from the brain contribute. Because more danger messages are occurring, the brain is less likely to utilize endogenous opioids to calm the system down.
From a survival standpoint this makes sense. In chronic pain, the future becomes less certain, and your top priority is to stay alive. If I can make you more sensitive to your environment, I can better protect you.
The body tells the brain when it is in pain: FALSE
Why – The brain is what produces pain. The body can only produce danger. The brain activates many areas in the pain experience, making pain multi-sensory. And the more this pain map is run, the more efficient your brain becomes at producing it.
Fun fact: The amygdala’s role in pain could be why females have more chronic pain than males.
The brain can send danger messages down your spinal cord that can increase the danger messages going up the spinal cord: TRUE
Why – If there are enough danger signals reaching the brain, the brain will want to know more; thus impacting the periphery.
Nerves can adapt by increasing their resting level of excitement: TRUE
Why – Action potential are key. Every nerve has a resting amount of activity, and a certain amount of stimulus is necessary before this action potential occurs.
When someone is extra sensitive, the nerves increase their resting excitement level so action potentials more readily occur. Adding more ion channels to less myelinated areas can further compound this sensitivity.
Fun fact – Ion channels change every 48 hours, and therapy can positively influence the change.
Chronic pain means an injury hasn’t healed properly: FALSE
Why – Read, like, everything I have ever written ever. Pain and injury are not the same thing. Tissues heal, tissues heal, tissues heal.
Receptors on nerves work by opening ion channels in the wall of the nerve: TRUE
Why – See above.
The brain decides when you will experience pain: TRUE
Why – Pain is a brain construct. Tissues can only send danger messages.
Fun fact – Laughing at a joke requires 5 different areas to be active in the brain.
Worse injuries result in worse pain: FALSE
Why – See video below
When you are injured, the environment that you are in will not have an effect on the amount of pain that you experience: FALSE
Why – Injuries and pain occur in an environment, not a vacuum. An ankle sprain may hurt on a sidewalk, but likely won’t if a bus is about the hit you.
Fun facts – Injuries in high stress environments are 7-8 times more likely to produce chronic pain. Also, kids who play contact sports early in life have less chance of developing chronic pain.
It is possible to have pain and not know about it: FALSE
Why – Pain is a conscious decision by the brain. No brain, no pain.
Nerves can adapt by making more ion channels: TRUE
Why – I already answered it duuuuude.
Second order messenger nerves post-synaptic membrane potential is dependent on descending modulation: TRUE
What did I just say? – I don’t know.
Why – The brain has the abilty to inhibit information coming up from the periphery via endogenous mechanisms. This is how placebo works.
Nerves adapt by making ion channels stay open longer: TRUE
Why – Because I said so…directly above. The brain will also make g protein ion channels, which can stay open for several minutes. This type allows for more danger messages to fire.
When you are injured, chemicals in your tissue can make nerves more sensitive: TRUE
Why – Much was previously mentioned, but the stress response plays a huge role here. When you go into a more sympathetic state, adrenaline, cytokines, and cortisol pump throughout the body. This change increases sensitivity of nerves throughout the body systems, and those in chronic pain are more geared toward this state.
Put it all together, and what do you got???
So with all the above information, we can see there are many misconceptions regarding pain. So it becomes very important to define what pain is. Here is a great definition:
“Pain is a multiple system output activated by an individual’s specific pain neural signature. The neural signature is activated whenever the brain concludes that body tissues are in danger and action is required.”
So Let’s Do Something about It
While we do need to know all the nitty-gritty regarding pain physiology, your patients and clients will not know what the heck you are talking about. Thus, you have to teach this information in a patient-friendly manner. Here were some of my favorite ways Adriaan used for TNE.
You can also mention to patients in chronic pain that one in three people keep their nerves elevated past normal healing times.
With this example, there are usually three questions that arise:
- How do you know this?
- Why did my nerves stay/become so sensitive?
- What can be done to calm them down?
Number one can be answered by the following points:
- You told me – it takes less activity for pain to arise.
- Your tests told me – physical exam and neurodynamic tests.
- Your doctor told – any anti-depressants or drugs like Cymbalta or Lyrica can calm the nervous system down.
We can answer number two by having them think about the many factors that could enhance sensitivity. These factors could be failed treatments, hearing different explanations, pain chronicity, life worries; basically anything that could make you feel threatened.
Number three is easily answered by explaining the powers of education, exercise, and medication.
The Old Speeding Bus Trick
Say you sprain your ankle. Would it hurt? How about if a bus was about to run you over? This tactic demonstrates that the brain makes a conscious decision as to whether or not pain should be experienced; and the greater threat always wins.
I Hate Having Neighbors
Here is a great way to explain spreading pain to patients.
Say your alarm goes off and you begin to feel pain. If your alarm stays on long enough, the noise may wake up your neighbors. If the neighbors stay awake because your alarm keeps going, eventually they will get agitated. It wouldn’t be surprising to see neighbors even farther away waking up if the alarm stays on too long.
You can also tie in the immune system in to this example. Immune molecules are like little police men that check out everyone and make sure the situation is okay. Nearby neighborhoods might also be checked out just to be safe.
The police watch the area until the problem is taken care of. But as is customary, a few months later the police may check-in to make sure everything is okay. This analogy can explain why pains you once had can reoccur.
The Road Often Traveled By
This analogy is a great way to show how chronic pain allows for neural pathways to turn on more efficiently.
Think of a neural pathway that would lead to a pain experience as a dirt road. If you get a lot of traffic along that pathway, eventually the road is going to have to get bigger to accommodate. So perhaps the road is widened. Maybe the next step is the road getting paved, then making the roads 2-laned, etc.
The more that pain pathways run, the more fluidly they do so. The pain experience is created faster and faster with the more traffic encountered.
The Top 5 Reasons Why a Bulging Disc Ain’t a Big Deal
You are inevitably going to run into someone who thinks having a bulging disc is a death sentence. Here are the 5 facts (in order) that you should mention to them:
- 6 weeks after a scan is performed bulging discs become smaller.
- You can get completely different results depending on the time of day the MRI was taken; early am is more likely to show disc bulges.
- Position MRI was taken in affects results.
- Levels that swell don’t move much; thus laying still or moving can impact results.
- 40% of asymptomatic individuals have bulging discs.
Two Lions Walk into a Bar…
This analogy is a great way to explain the stress response. Imagine you are watching television minding your business when a big African lion walks in the room. What happens to your body systems?
- Adrenaline pumps through the bloodstream, increasing heart rate, breathing, alertness, etc.
- Big strong muscles turn on; smaller muscles turn off.
- Raise voice and speak short and sharp.
- Shallow and fast breathing.
- Digrestion slows.
- Memory fogs.
- Reproductive systems stop (unless you dig lions)
- Many other things.
When the lion leaves the room, the body returns to its previous resting state. Chronic pain states is akin to having this lion following you at all times. This state, which can be perpetuated by many factors, can keep the above changes going relentlessly. Our goal with therapy, is to make that lion less threatening.
Strategize
While we have been exposed to great science and metaphor, the practical component was what did it for me. Adriaan had so many wonderful suggestions for implementation that I had to list some of my favorites:
- Train the entire staff on TNE; including front office.
- Designate particular days as TNE days.
- Can teach in 10 minute increments.
- Carefully use the word pain. Asking patients pain rating repeatedly may increase pain ratings.
- Have a strict cancel/no show policy: Adriaan likes one cancel; >10 minutes late leads to a reschedule.
- No more than 5 exercises for HEP.
- Aerobic exercise is huge for chronic pain. Perform at >50% VO2 max and >10 minutes.
A big one for me regards coping skills. Before a patients calls in on a bad day to see a therapist, 5 strategies should be performed first:
- Problem solve – find a cause/relationship.
- Ice/heat/TENS.
- Perform your exercises.
- Get away – walk for a little bit, then relax and take a cleansing breath.
- Do not cancel all activities. Do as much as you can.
Quotes from Adriaan
- “Light a candle, watch Oprah.”
- “The holy grail to chronic pain is prevention.”
- Take that patient. Own that patient. Fight for that patient.”
- “Your challenge is to be so good a these [chronic pain] patients that the other stuff will become mundane.”
- “If you are a PT and have not had back pain you are dead to me.”
- “Aerobic exercise is gold standard for chronic pain.”
- “Parenting sets up pain later on.”
- “The biggest boost for the immune system is social interaction.”
- “Low back pain is the common cold of the musculoskeletal system.”
- “Your job is to make your patient so smart that pain decreases.”
- “30% of pain is insidious onset”
- “You are not treating evidence, you are treating a patient.”
- “The best clinical question you can ask is ‘what do you think is going on with your x.’”
- “Pain protects.”
- “Make patients responsible for their own care.”
- “The bigger threat wins.”
- “The biggest predictor of chronic pain is acute pain.”
- “pain spreading is an expansion of receptor fields.”
- “When pain is involved motor control becomes 2nd.”
- “Pain is a unique human experience.”
- “If you live your pain, you become very good at living your pain.”
- “Don’t forget the human being.”
- “You are a walking placebo pill.”
- “Lyme disease is the new fibromyalgia.”
- “A brain that doesn’t know is the most dangerous thing on the planet. Make the unknowns known.”
- “Pain is what I think.”
- “You own your pain.”
- “If you teach about pain and they feel worse, you got them.”
- “Chronic pain patients are not weak, they are deconditioned.”
Wow….> 1,000 followers! Nice job ZC! Keep it up.
Thanks for your support Aline. You rock!
Hey Zac,
I was reading http://courses.washington.edu/conj/sensory/pain.htm which may very well be outdated, but it says that C-fibers are unmyelinated. Can you speak to this?
Thanks!
-Andy
I am not sure if you are familiar with this textbook, but in “Pathology: Implications of the Physical Therapist” by Goodman and Fuller, there is a section that states pain fibers have no myelin covering. I just want clarification on this topic and figured you could help me.
Thanks again,
Andy
Hey Andy,
Great question. C fiber axons have a very small filament surrounding them called Schwann cells; these guys form myelin. These cells surround the entire peripheral nervous system, so there truly are no unmyelinated nerves in the body. It’s a technicality issue; the sheeth is nowhere near as thick as A and B fibers to the point where it’s practically unmyelinated.
Found a reference here http://www.getbodysmart.com/ap/nervoussystem/supportcells/unmyelinatedaxons/tutorial.html
I can also shoot Adriaan an email to see if he has a better reference.
Just goes to show you can’t trust a book that calls them pain fibers 🙂
Hope that helps,
Zac
That’s what I figured. A covering so thin, it’s “negligible”, but still exist nonetheless. And I definitely trust you on the topic, but if you do hear back from Adriaan with another reference, please let me know.
I also would like to thank you for all these notes. They are just inspiring, informational, and overwhelming (as a student). It’s just astonishing how far you’ve come in the short amount of time you’ve graduated. As a student, I feel so far away from where you are and want to attack all of this information, particularly PRI. However, PRI is just so complex and it’s simply too much to attach both school and PRI at the same time. I have about a year and a half left of school. How do you think I should go forward? Should I start the home-courses while in school? During clinicals? Or should I finish school and then start it?
Your stuff is great and it’s inspiring to know there’s so much more and so much better out there beyond school.
Thanks in advance!
Andy Pham
I shot Adriaan an email so I’ll let you know 🙂
I appreciate your kind words and humbled that my writing inspired you. It is a lot to take in especially when it is so foreign to what is being taught in school.
I did almost all of my studying after PT school, but if I knew about it before that I would’ve taken advantage of the nice student discount you have. I would do the home courses to at least have the terminology down; the more exposure the better. It will actually help you quite a bit with your anatomy/kinesiology knowledge. It will also make you hate PT school. Still worth it.
Any way I can facilitate your learning process let me know,
Zac
Hey Zac,
Love your blog. In regards to aerobic exercise being the gold standard for chronic pain, any stuff you recommend reading about that more? I’ve always heard just exercise in general. Why aerobic specifically?
Thanks1
Hey Brent,
Appreciate the kind words.
Any of the books that Adriaan has put out discuss this a bit more in-depth. Aerobic exercise helps increase general bloodflow as well as BDNF production (for neuroplasticity). Nervous system tends to calm down when movement, space, and bloodflow are present. Higher level activity (anaerobic) is a bit more threatening to an individual due to the intensity.
I may be able to dig up some articles for you, but I think a bulk of the aerobic exercise research has been done on people with fibromyalgia. If you search fibro and aerobic exercise you are bound to find some research.
Hope that helps,
zac
Awesome, thanks Zac!
Hey Zac –
Great blog! I am reading Explain Pain and your blog helped clarify and summarize many of the concepts. I am new to TNE but it sounds right up my alley. Any books you’d recommend?
Thanks,
Jessica
Hey Jessica,
Great to hear from you and thank you for the kind words.
There are several books I would recommend.
Therapeutic Neuroscience Education by Adriaan Louw
The Sensitive Nervous System by David Butler
Any book by the NOI group
Topical Issues in Pain Series by Louis Gifford…He also has some new ones out that I haven’t read.
That should be a healthy start 🙂
Keep learning and stay in touch,
Zac
[…] very important point to make, and this goes for all injuries is that pain does not equal injury. There have been several cadaveric studies that demonstrate nerve damage or compression in people […]
[…] Educate, educate, and educate. We must let our patients know that pain does not equal […]
[…] Addressing fear of pain and reinjury. […]
[…] first goal addressed in education is making the patient understand pain. Patients must realize that pain is the defender, not the offender. It is our body’s way to […]
[…] pain can reduce the threat value and improve pain management. And the good thing about explaining pain? Research shows that it can be an easily understood […]
[…] on what Butler’s group and the research says as of right now. Based on what I have learned from Adriaan Louw, having any of the following is what constitutes a positive […]
[…] Educate on the whole problem to include tissue health status, the nervous system’s role, and test […]
[…] body’s alarm system alerts us to danger or potential danger. This alarm system is composed of sensors throughout the body, the eyes, nose, and ears. It is these sensors that are our first line of […]
[…] overcoming pain. Instead of no pain, no gain, the authors like to use “know pain, or no gain.” Understanding pain is essential for squashing fear of pain, which leads best toward the road to […]
[…] will usually educate the patients to some degree on pain physiology, followed by whatever objective impairments I find that can improve upon one’s complaints. In […]