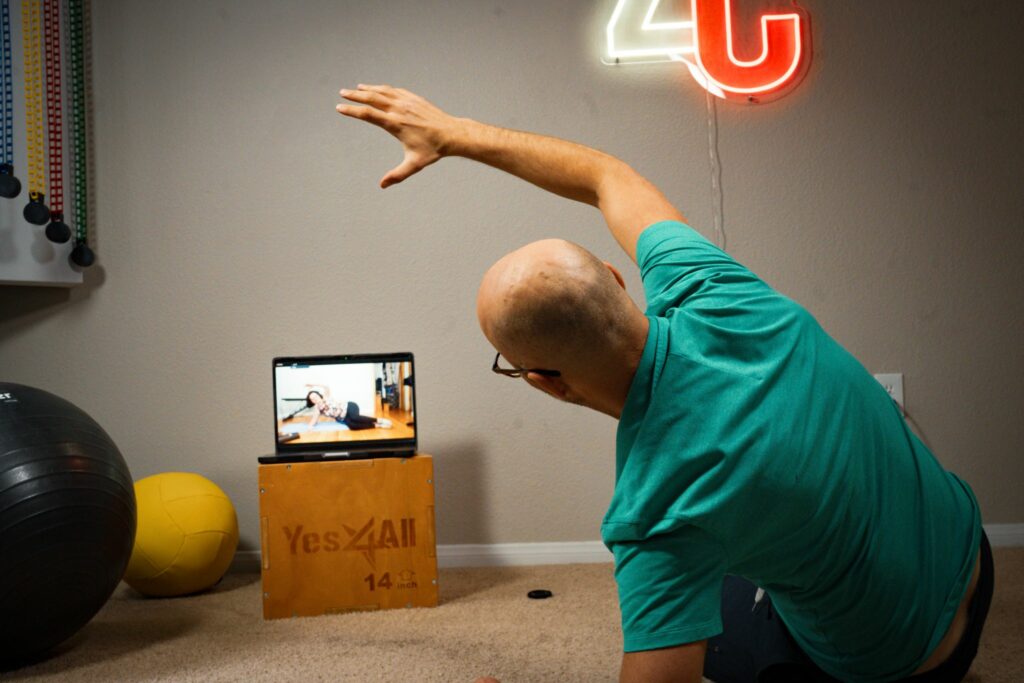
Better movement. Less pain.
Move better, hurt less, train smarter–with a customized plan, ongoing video feedback, and a coach in your corner.

Master biomechanics. Coach smarter.
Clear decision-making, better exercise selection, happier clients–with a simple framework you can apply Monday.
Real People, Real Results
Back to training clients pain-free after 8 failed PTs and $30k in treatments
Deadlifting pain-free again after years of chronic hip pain
Hip pain gone after months—now coaching with better movement