Table of Contents
When I think About You…
Prompted by some mentee questions and blog comments, I wondered where manual therapy fits in the rehab process.
To satisfy my curiosity, I calculated how much time I spend performing manual interventions. Looking at last month’s patient numbers to acquire data, I found these numbers based on billing one patient every 45 minutes (subtracting out evals and reassessments):
- Nonmanual (including exercise and education) = 80%
- Manual = 20%
- Modalities = 0%!!!!!!!!!!!!
Delving a bit further, here’s my time spent using PRI manual techniques versus my other manual therapy skill-set:
- PRI manual = 14%
- Other manual = 6%
As you can see, I use manual therapy a ridiculously low amount; skills that I used to employ liberally with decent success
There’s a reason for the shift
I want my patients to independently improve at all cost and as quickly as possible. The learning process is the critical piece needed to create necessary neuroplastic change; and consequently a successful rehab program.
Rarely is learning involved in manual therapy.
Manual therapy at most should provide a salient stimulus that facilitates a positive learning environment for that individual.
Despite my minimalist manual approach, I think it is still important to have a vast skill-set to skin the proverbial cat. The more novel inputs one can provide, the more likely many patients will enter that aforementioned learning environment.
Here’s how I select what I am using.
So I’m Kinda Biased
Before we dig into what I like to use, here are a couple biases I am going to make:
#1 All manual techniques likely work under a similar mechanism.
Under the right context and for the right individual, every technique works. You are not breaking up scar tissue, deforming fascia, and all this other hullabaloo.
Remember, its about providing a salient stimulus that coaxes the nervous system into creating a favorable novel learning environment.
#2 Patient preference trumps everything
This reason is why you might need a “toolbox”. One technique is not going to work for everyone. Some patients may prefer certain types of touch compared to others.
Some people want you to be gentle, some dig stretching.
Believe it or not, some people want manual therapy that is uncomfortable.
Whatever the patient wants, insofar that it meets your mutual goals, is what ought to be done.
What are those goals?
Goals? I’m Glad you Asked
From here on out, let’s assume the patient has no intervention preference. Here are my goals with my manual interventions.
#1 – Can it change my PRI tests?
You can have a toolbox that Tim Taylor would envy, but you will be unsuccessful if you lack a systematic approach. You can’t always expect to hit a bull’s-eye randomly throwing darts at the neural dartboard.
A system provides an objective end-game to which your manual interventions ought to change. It doesn’t rely on patient perception, which can often be clinically misleading and send you on a pain scavenger hunt.
My system is PRI, and my primary goal with that system is to restore movement variability. I’ll define that as active and passive mobility in three planes. You can use whatever system you like, just have something.
#2 – Can it ameliorate the patient’s symptoms?
If pain remains after a patient’s movement variability is restored, you might need a symptom-reducing input. Pain does impact motor control, and a well-planned manual intervention followed by movement can have quite the positive impact.
Other Considerations
Preference, objective measures, and patient perception take top priority. However, there are a few other important qualities to consider when selecting a manual technique:
- Speed – The less time I have to spend doing a technique the better. Speed allots patients more time to learn a movement or concept.
- Comfort – I will generally perform the most comfortable intervention possible. Throwing pain in the mix runs the risk of increasing threat perception.
- Skill level – I usually pick stuff I am good at. You ought to do the same.
The Brand Names
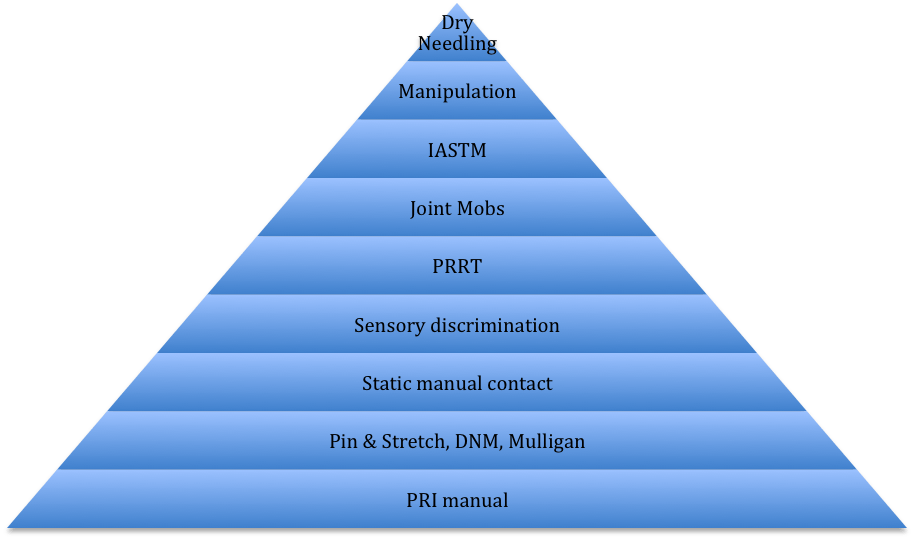
I have accumulated many manual skills over the years. There are certain body regions that I find certain techniques more effective than not, but In general my hierarchy goes like so.
Bottom is most frequent, top is least frequent.
Let’s dive a little deeper if you are unfamiliar with each. I’ll rate the following qualities:
- Movement Variability
- Symptom relief
- Speed
- Comfort level
- Best body regions
Here’s the grading scale, from least to most effective:
Least effective Most effective
Hella lame ⇔ Yuck ⇔ meh⇔ mmk⇔ Nice!⇔ Hellz Ya⇔ Daaaaaaaamn
Let’s break it down
PRI Manual
- Movement Variability: Daaaaaaaamn
- Symptom relief: Daaaaaaaamn
- Speed: mmk
- Comfort level: meh
- Best uses: First line of defense, thorax, neck, cranium, hips
Obviously quite biased toward these techniques. These are hands down the best at improving variability; especially because they have a motor learning component. The only downside is the discomfort that comes with playing on ribcages. Sometimes you can feel like you are suffocating during. But because it’s most often not the problem area, my patients generally like it.
Learn it here.
Pin & Stretch
- Movement Variability: mmk
- Symptom relief: Hellz Ya
- Speed: Hellz Ya
- Comfort level: mmk
- Best uses: Hip, shoulder, spine, neural tracts
Have not had formal training, so I can’t say what it’s based off of (hint, it rhymes with K-mart spree). Basically, take up tension, and move through that tension. I have modified my contact over the years to make this technique as comfortable as possible; adjusting if my patients perceive any pain.
Dermoneuromodulation (DNM)
- Movement Variability: Yuck
- Symptom relief: Hellz Ya
- Speed: meh
- Comfort level: Daaaaaaaamn
- Best uses: post-op, extremities
I’ve taken quite a liking to Diane Jacobs’ technique because it is quite comfortable. I use it most often after I’ve maximized one’s movement variability and if symptoms remain. I find it a nice finisher to most sessions.
Learn it here.
Mulligan
- Movement Variability: mmk
- Symptom relief: Hellz Ya
- Speed: Nice!
- Comfort level: Daaaaaaaamn
- Best uses: Neck, elbow, knee
Have not had formal training, but my musculoskeletal professor in PT school was a big fan and taught us a lot. Basically, Mulligan boils down to changing the context at an area, then having the patient move within that context. I love Mulligan because it’s fast, painless, and has a learning component to it. You can also take these techniques home with you. Winner for me on many levels.
Learn more here.
Static Manual Contact
- Movement Variability: Nice!
- Symptom relief: Nice!
- Speed: Yuck
- Comfort level: mmk
- Best uses: Post-operative stiffness, frozen anything
I use this style on my peeps who have shoulder surgery. I find that combining low load long duration with gentle manual contact to be quite an effective way to explore movement when passive restrictions hold the patient back. My contact usually goes over muscle areas that make sense. For example, if someone is limited in external rotation, I’m touching the subscapularis region. You can also throw neural flossing into the mix. It’s quite versatile; just takes a while.
Sensory Discrimination
- Movement Variability: Hella lame
- Symptom relief: Nice!
- Speed: Meh to nice!
- Comfort level: Hellz ya
- Best uses: chronic pain, post-operative sensitivity
I’ve been using this stuff a lot more since I read Adriaan Louw’s CRPS book, and this stuff works. I like it quite a bit because it keeps the patient active in treatment. It’s almost meditative. Great things happen with this post-operatively.
Primal Reflex Release Technique (PRRT)
- Movement Variability: mmk
- Symptom relief: mmk
- Speed: Daaaaaaaamn
- Comfort level: Daaaaaaaamn
- Best uses: craniocervical region, shoulder
PRRT is a crapshoot for me. When it works you will dazzle your patients; when it doesn’t you will look like an ass hat. It can have profound mobility effects on the entire body, and probably works best with RTMCC people who may not need integration. Sadly the effects don’t last super long. At least it only takes seconds to perform.
Learn it here.
Joint Mobs
- Movement Variability: Yuck
- Symptom relief: meh
- Speed: mmk
- Comfort level: Nice!
- Best uses: Hips, knee (especially post-op), ankle
Maitland was God in PT school, but I just haven’t found this stuff to be super effective. It might be a nice homuncular refreshment for certain people, but I wouldn’t expect miracles. And for the love of David Butler stop worrying about grades. You’re not affecting tissue properties.
Instrument Assisted Soft-tissue Mobilization (IASTM)
- Movement Variability: Hella lame
- Symptom relief: mmk
- Speed: mmk
- Comfort level: Nice!
- Best uses: edema reduction, post-operative
I don’t use this jazz too often, as I feel there is probably a better social-grooming/neural component when there is actual physical contact between people. That said, it’s a novel stimulus that occasionally works. Please don’t bruise people and don’t make it hurt. Pick whatever tool is cheapest; doubt there is much difference among them all.
I learned it from Dr. E.
Manipulations
- Movement Variability: mmk
- Symptom relief: Nice!
- Speed: Hellz Ya
- Comfort level: meh
- Best uses: feet, neck pain, ankle sprains
“When in doubt, manip it out” was the mantra in my residency, but it has fallen out of favor with me over the years. There are just many less threatening techniques that work just as well. I will say this though; thrust manips on the feet work wonders.
From what I’ve heard, the most gentle of the bunch is through Gibbons and Tehan. I am also curious about SMI‘s extremity offerings.
Dry Needling
- Movement Variability: ???????
- Symptom relief: ????????
- Speed: ?????
- Comfort level: Hella lame
- Best body regions: ?????????
I haven’t really figured out where this sits for me yet, so I’ll reserve judgment right now. None of my patients have been needled yet, and the folks who I think it may help have needle-phobias. Perhaps if I update this a year from now we will have some answers.
Take it through SMI.
The Last Word
These techniques make up my 20%. As long as you respect patient preference, maximize movement variability, and have patient independence on the mind, you are doing the right thing.
You don’t have to pick the stuff I use. The best advice I can give when learning manual interventions is to pick skills that you feel you can perform well, and use them as an adjunct to a non-manual-dominant program.
Thoughts or comments? What manual interventions do you use? Where does manual work fit for you? Comment below.
