We pursue health by attempting to optimize many qualities—movement, power, endurance—but these are just a few of the qualities needed to be healthy.
How often do we look at optimizing all of our physiological systems?
That’s where functional medicine became an area of interest for me. I was dealing with some health issues over the last couple years, and I sought out Ben House with great success. I was curious to learn more about this discipline, so I attended his retreat and went through his mentorship; learning a great deal in the process.
It was at Ben’s retreat that I got to listen to Bryan Walsh, and was blown away.
For those who don’t know, Bryan is a naturopathic physician who is a an absolute Jedi with understanding and designing treatments from physiological mechanisms.
Bryan took us through an intense physiological journey over those few days, and I absolutely needed more. Thank the maker that Bryan announced his two day seminar.
And boy did he not disappoint.
Over two days I drank from the firehose of all things blood chemistry and functional medicine. The amount of research we went through was astounding, both on lab values and interventions. I was amazed at how many simple treatments could have profound effects on many common conditions we see people developing.
This course contained useful protocols involving supplements, optimal lab ranges based on reducing all cause mortality, and so much more, but to list the exact to-dos would be a disservice to both Bryan and you. Moreover, given my inexperience with functional medicine, I wouldn’t feel comfortable telling you where you should start with someone. Appraising lab work is serious business, and likely requires more coursework beyond what was taught here.
What I do feel comfortable with though, is showing you just how impactful our bread and butter can be: exercise, sleep, nutrition, etc. Hammering these basic practices can lead to substantial changes on a blood chemistry, and my hope is that this review gives you a different lens to view all the wonderful things you do as a clinician and/or coach.
If you want to learn more, I have the strongest recommendation for everything Bryan has to offer. If you want to beef up your understanding of physiology, and learn how to practice a functional medicine approach with your clients, he is by far one of the best you can learn from. I recommend signing up for all of his courses as I have, and you can find that here.
Table of Contents
THE FUNCTIONAL MEDICINE (+FAMILY) TOUR
Let’s dive in.
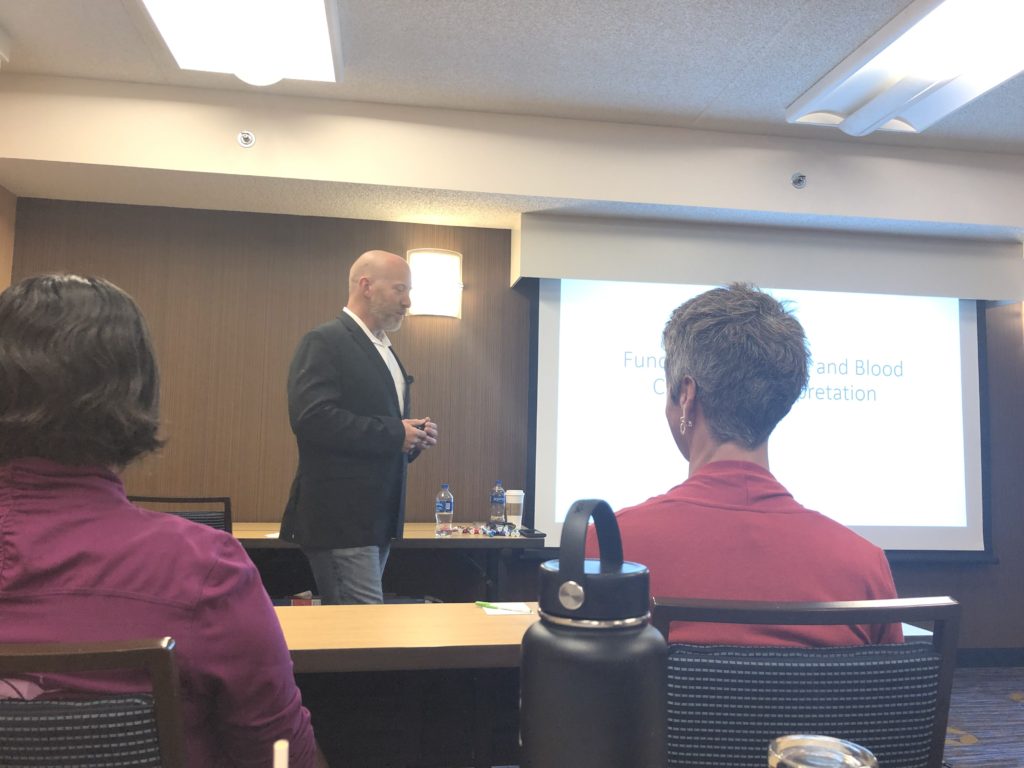
Functional Medicine and Blood Chemistry Interpretation
Blood chemistry, the stuff you get from a blood draw, is arguably one of the most important and undervalued diagnostic test we have at our disposal.
The functional medicine waters have sadly been muddied by fancy tests that have yet to be validated. This shift has come at the expense of appreciating a simple blood chemistry, which surprisingly has a vast amount of research on its explanatory power and links to all-cause mortality.
Blood chemistry is accurate, used worldwide, respected, and inexpensive. It can evaluate the physiology of multiple systems and provides information that can easily direct both interventions and further diagnostics.
Where conventional medicine uses these markers to treat pathological lab values, functional medicine focuses on optimization; maximizing health versus ensuring survival. Both disciplines have a purpose.
Yet how are these “optimal” ranges determined? Most sources list a supposed optimal value without explanation or evidence.
That’s where Bryan shines. Bryan’s literature scour focuses on those ranges which are associated with the lowest all-cause mortality. You’d be surprised at how often Bryan produced studies that showed certain low/high normal lab ranges linked to increased cardiovascular incidents if people had certain low or high normal lab ranges. Hence the need for optimization.
Seeking optimization might be what we need to maximize health and longevity.
Glucose
Glucose is the primary substrate for ATP production within the cell. In order to support ATP production, a certain amount of glucose ought to exist outside the cell; ready for use when the time comes.
It is this extracellular glucose that is measured on a blood chemistry, serum glucose. These levels are determined by food intake glycogenolysis (glycogen breakdown), and gluconeogenesis (formation of glucose in the liver from other compounds).
Serum glucose ought to stay in a pretty tight range both at fasting and post-meal (postprandial) levels. Dipping too low or high can have deleterious consequences within the body.

Glucose and Hormones
Several hormones tightly regulate glucose. As glucose values rise, insulin activates to put that sugar in your donut to work.
Insulin stimulates glycolysis, glycogen (stored glucose) synthesis, cholesterol synthesis, and lipogenesis (fat formation). Putting glucose to work like this allows serum values to drop back down to their homeostatic norm.
Surprisingly, insulin is released before glucose has a chance to enter the bloodstream. Incretins, GLP-1 and GIP are the gut hormones that make this possible. These hormones kick in within two minutes of glucose ingestion, priming the body for glucose utilization. This mechanism is considered the first phase insulin response, which both limits glucose elevation after meals and suppresses liver glucose production. Dysfunction within this response can be one of the earliest type 2 diabetes markers.
The second phase insulin response is when insulin synthesis and release continues until serum glucose is normalized.
While insulin is the only hormone that lowers serum glucose, there are four different ones that raise this value: glucagon, growth hormone, cortisol, and epinephrine.
The intent would be to have balanced activity among these hormones. It seems according to Bryan’s research, a serum glucose between 80-85 mg/dL fits the bill. High normal values above 85 mg/dL have been associated with higher mortality values.
Glycemic Variability
No, this isn’t the cool kind of variability. Glycemic variability is where serum glucose levels go to extreme highs and lows after eating. Glucose can shoot too high if the body’s two insulin responses fail to work properly. Conversely, serum glucose can be too low if excessive insulin or GLP-1 production occurs.
Neither of the above two scenarios are desirable, as large glycemic swings are associated with increased oxidative stress, hypoglycemic tendencies (shakiness, lightheadedness, irritability, poor quality of life, obesity), and so much more.
You are better off having high, stable fasting glucose than you are glycemic variability.
Restoring Glucose Utilization
To normalize the body’s interaction with glucose, the focus is on increasing glucose disposal while simultaneously decreasing fasting glucose. Objective markers that focus on these qualities include Glycomark (2 week postprandial glucose response, the most important), C-peptide (an insulin secretion measure), and Hemoglobin A1C (2-3 months of blood sugar changes).
While there are tons of supplements and herbs that can help one reach these glucose goals, I’m more interested in showing how the things we are already doing—exercise, mindful eating, etc—can positively impact these functions.
Chewing more can significantly improve both glucose disposal and fasting glucose. Yes, chewing.
Regardless of body type, completing 40 chews per bite (versus 15) decreases energy intake, lowers postprandial ghrelin (hunger hormone), and increases postprandial GLP-1 and cholecystokinin. All of these factors aid in normalizing the glucose levels after eating.

Exercise can also improve glucose disposal by increasing insulin sensitivity, mitochondrial function and biogenesis, and intracellular glucose utilization.
As for diet, focusing on mitochondrial support is essential. If your glucose utilization is whack, consider a diet that is low in carbohydrate, moderate in protein, and contains copious amounts of vegetables.
Lipids
Fat metabolism involves breaking down triglycerides into useable substrates for the tissues. The first action on this pathway is lipolysis. This is where the pancreas breaks down triglycerides into fatty acids and beta monoglycerides.
Fatty acids and beta monoglycerides then aggregate with bile acids, forming larger structures called micelles. This new structure now has the ability to pass into the membrane of the jejunum.
Once in the jejunum, the micelles split again into triglycerides and beta monoglycerides, only to recombine into triglycerides.
Now that these triglycerides are repackaged in a different location, they can combine with cholesterol, phospholipids, and beta lipoprotein to form chylomicrons. These molecules allow for fat transport to occur to the tissues via the lymphatic system.
[Side note: Want to see a dope video on fat metabolism? Check it out here]
Understanding fat metabolism provides the framework for how and why we look at a lipid panel on blood chemistry. This panel tests the cholesterol associated with the lipoprotein particles, with chylomicrons being one of several lipoprotein subgroups. Others would be VLDL, which hands off fat to the body; LDL, which is basically VLDL without the fat; and HDL, which cleans up fat in the periphery and transports it back to the liver.
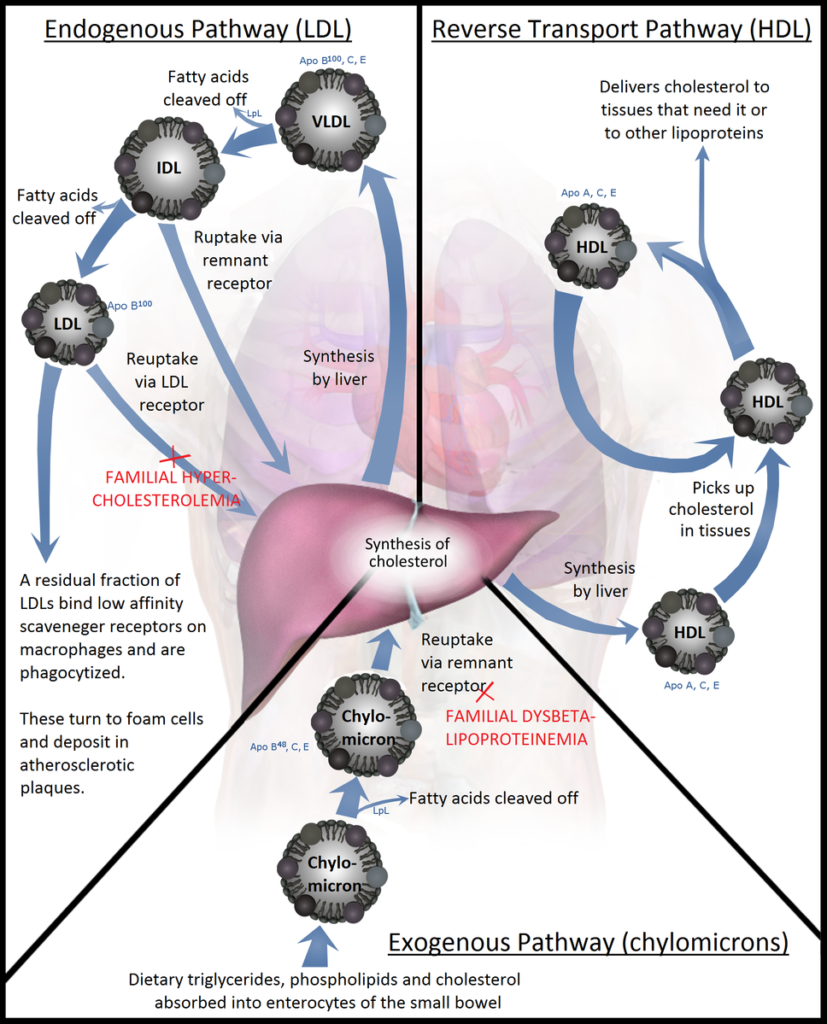
Total cholesterol amount is not as impactful as we once thought. It seems as though lipoprotein particle number is more predictive for cardiovascular disease risk. Thus, having optimal values for LDL, HDL, and triglycerides likely reduces cardiovascular disease risk.
Out of all the measures, HDL was conventionally thought of as the “good cholesterol,” but this is far from the case. HDL can have both pro and anti-oxidant functions; either helping or promoting oxidative stress.
If HDL is too high or greater than LDL, there is an increased risk of coronary heart disease. HDL will spend more time mopping up lipopolysaccharides (LPS), which are compounds that promote inflammation. When HDL spends time focusing on LPS removal, HDL no longer acts as an antioxidant and elicits greater oxidative stress. This switch in function is correlated with leaky gut.
If you have high LDL and normal HDL, you are likely healthy AF. How to make that happen? Check out Bryan’s course!
Complete Blood Count
This section focused on oxygen delivery to cells—aerobic metabolism.
Normally, aerobic metabolism occurs by the krebs cycle and electron transport chain running efficiently within the mitochondria. A healthy aerobic system both creates energy for the cell and manages pH.
Aerobic metabolism requires oxygen, which comes to the cell via hemoglobin in the red blood cell. There is a certain amount of hemoglobin necessary to keep cells healthy. If hemoglobin levels drop too low, cells will not receive adequate oxygen, and problems will ensue.
Hypoxia (lack of oxygen) causes complexes within the electron transport chain to stop working, slowing the krebs cycle down.
Pyruvate, the molecule which starts the krebs cycle, converts into lactate, which increases hydrogen ion concentration within the blood. This shift increases pH acidity, which alters enzyme function. If your enzymatic function is negatively impact, so is your cellular function. Aka, you have problems.
Given just how vital oxygen is to our body, we probably want the oxygen delivery method to be on fleek. We want healthy red blood cells. Lacking healthy red blood cells is called anemia, to which there are a wide variety of causes (you learn them all at Bryan’s course).
While there are many measures that provide insight into red blood cell health, hemoglobin, the oxygen carrier, is one of the most important.
Many nutrients are needed to produce hemoglobin: vitamin C, copper, iron, zinc, vitamin B6, and protein. Seeing this list of nutrients ought to illustrate the far-reaching effects of a diet high in vegetables and healthy protein sources! Deficiency in any one of these nutrients, not just iron, could lead to anemia.
Infection
Infection is likely something that is going on within our bodies more than we think. Arthritis and many common chronic diseases may have had an infection trigger the disease cascade.
Your blood contains dormant bacteria that can be resuscitated given the right circumstances. One common circumstance that can make one infection-prone is iron dysregulation. Iron is like chocolate for bacteria. Excessive iron production may cause dormant bacteria to awaken, releasing lipopolysaccharide in the process. Lipopolysaccharides can cause low-grade inflammation, contributing to many bodily issues.
Though we mentioned anemia can be caused by many factors, iron’s relationship to bacteria ought to make you rethink simple iron supplementation for anemia. Perhaps anemia is a protective mechanism for an ongoing infection; illustrating blood chemistry’s complexity and the need for thorough professional examination.
Assessing for Infection
Immune cell concentrations are the key to determining if our body is battling an infection.
White blood cell count is the first measure to consider, as it can tell you the infection chronicity. This measure will be high with acute infections, low in chronic.
To determine the specific infection, we have to dig way deeper. We have to look at each specific white blood cell, as each has a specific action:
- Neutrophils: high in bacterial infections and inflammation
- Lymphocytes: High in viral infections and autoimmune disorders
- Monocytes: High in systemic inflammation
- Eosinophils: High in late stage inflammation, allergens, and parasitic infections
- Basinophils: High in general inflammation and hypersensitivity
- Platelets: High with hemolytic anemia and cardiovascular disease; way high may be present in cancer
There are many different herbal and conventional routes that can impact infection once diagnosed, many which Bryan goes through in his course.
Inflammation and Cell Damage
Inflammation has wide-ranging effects on blood chemistry. There are several reactants that are altered when inflammation is present, but the big two to measure are erythrocyte sedimentation rate (ESR) and c-reactive protein (CRP).
ESR and CRP
ESR looks at how fast red blood cells settle to the test vial bottom. Inflammation makes red blood cells stickier, slowing their downward movement. This value is often high with autoimmune diseases and infection, and responds more chronically.
CRP, on the other hand, responds to acute inflammation. It is produced by the liver as a consequence of cytokine production.
Viewing the relationship between these two markers can provide several insights. High CRP with minimal ESR change signifies an acute infection. High ESR without CRP change shows there was an insult two weeks before the draw. And if both are high? You likely have an inflammatory process underway.
AST and ALT
Aspartate transferase (AST) and alanine aminotransferase (ALT) are popularly paired together to measure inflammation.
In the past, AST and ALT ratios were used to measure liver function, but current research shows that these markers are worthless at estimating liver health. All is not lost though, as AST and ALT may be useful inflammatory markers.
AST is an enzyme in the liver, heart, skeletal muscle, pancreas, kidneys, and gonads. It is present in the cytosol of red blood cells and cardiac muscles, and in the mitochondria of hepatocytes. It functions with amino acid synthesis and metabolism. If high, there is likely active tissue and cellular destruction.
ALT is highest in the liver, but is also present in the heart, muscles, and kidneys. High-normal ALT has been found in those with metabolic obesity and atherosclerosis.
Liver Health
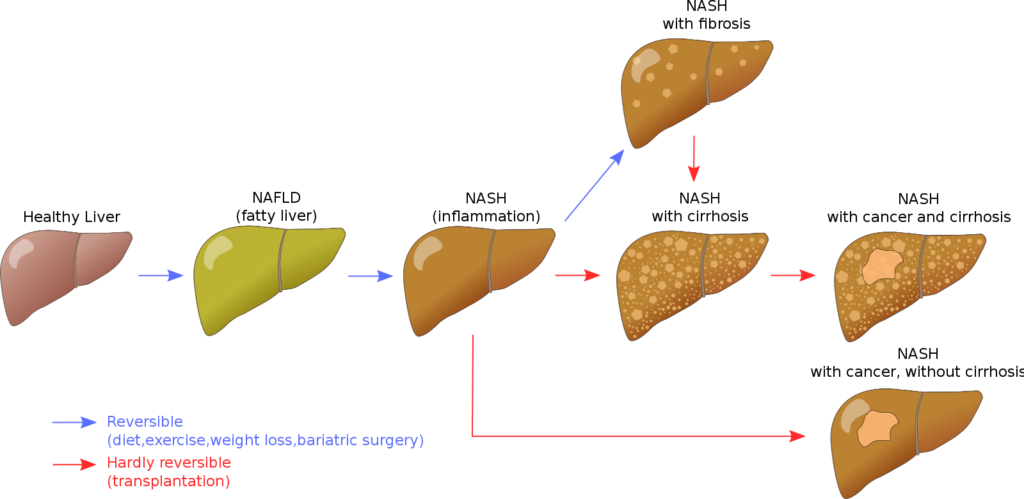
If AST and ALT aren’t so great at measuring liver health, then what is? Here we can look at bile acids and the fatty liver index.
Bile Acids
Bile acids form when cholesterol makes a conversion as it enters the liver. These acids participate in a conjugate reaction with glyciene and taurine to convert to bile salt.
Bile salt is active in fat emulsification, the break down of trigylcerides by pancreatic enzymes. Once fats emulsify, they can be absorbed in the small intestine and assist in the removal of cholesterol, hormones, and toxins. Thus, healthy bile acid amounts mean healthy fat metabolism.
Typically, bile acids were only measured if cholestasis was suspected during pregnancy, but it’s actually a great early measure for liver dysfunction. If bile acids do not convert to bile salt, fat digestion will be impaired, and subsequently liver health. Thus, bile acids will increase before any changes in ALT, AST, or bilirubin occur. This mechanism can be disrupted by glyciene deficiency, bacterial overgrowth, and xenobiotics to name a few culprits.
Fatty Liver Index
Aside from bile acids, the fatty liver index may be one of the better markers for those with liver dysfunction.
As mentioned previously, AST and ALT fail to detect fatty liver. Fatty liver comes in patches, yet biopsies only evaluates 1/50th of the liver. We need better measures.
That’s where the fatty liver index comes in. Considering that 30% of the population has fatty liver (and 90% of the obese population), we can look at body mass-related values to see if one is impacted. These values measures would be BMI, waist circumference, triglycerides, and GGT.
You can calculate your Fatty Liver Index here.
Detoxification
There is no woo-woo here. You may think that lead, mercury, and arsenic are the clear bad guys to worry about, but consider that there are over 100,000,000 million chemicals in existence. The World Health Organization estimated in 2011 that 4.9 millions deaths and 86,000,000 disability-adjusted life years can be attributed to environmental chemicals.
Negative effects can be seen even in small doses, especially in cases of persistent exposure. If chemicals are ingested and we cannot excrete them, there can be alterations in organ function, nutrient absorption, polymorphism production, and toxin interference with cellular processes.
The higher levels one has of xenobiotics, the lower the basal metabolic rate, beta oxidation, and so much more. Worst case scenario? Development of diabetes, infertility, cancer; the list goes on.
Though we all likely contain toxins, all is not lost. Xenobiotics will leave the body if a gradient exists. What we must do is create this gradient.
The Detoxification Pathway
Toxins are likely stored within our fat cells. Thus, emphasizing fat loss while supporting our bodies own detoxification process can help us clear toxins, and improve our health.
In order to support detoxification, we must first learn how it works. Detoxification occurs predominantly in the liver across four phases.
Lipolysis must first be induced, causing the xenobiotic to leave the fat cell and enter the bloodstream. From there, the four phases of detoxification can take place:
- Phase 0: Xenobiotic enters a liver cell through the bloodstream
- Phase I: A hydroxl group (-OH) attaches to the xenobiotic
- Phase II: The xenobiotic undergoes a conjugation reaction with glutathione or another compound
- Phase III: The xenobiotic leave the cell
Supporting Detoxification
In order to support detoxification, we must utilize interventions that include xenobiotic mobilization, liver detoxification support, and excretion promotion.
Though Bryan recommends specific foods (e.g. many cruciferous vegetables) and supplements (e.g. rooibos tea) to support each phase, exercise, calorie restriction, and sauna use are three modalities that impact almost every detoxification phase.
I won’t get into detail with each specific supplement Bryan recommends. That’s where I’d check out his awesome detox program.
Purpose
My favorite lecture of the seminar, Bryan research-bombed us mindset’s impact on the body. Consider that self-rated health is an independent predictor of mortality, increasing lifespan by 7.5 years alone!
What about those with dispositional pessimism (everything is wrong)? This outlook correlates with shorter telomere length and higher inflammatory markers. Whereas increased optimism has been associated with decreased respiratory disease, heart disease, infection, and overall mortality risk.
All that being said, positive thinking in and of itself doesn’t work. Fantasizing about the future saps energy, and being positive cannot be forced.

What is more effective is tying your life to a bigger purpose. Purposeful individuals live longer and have decreased disease risk.
Social Isolation
What if I told you that immunity and inflammation are intimately linked to your social community or lack thereof? In fact, the activity of these systems depends on it.
In caveman days, we lived in a tribe. Other people carried germs, so an exceptional immune system was needed to fight infections. The inflammatory process is useful if injured, but life-threatening injuries are less likely in groups. Others can take care of us when we are hurt. Thus, inflammatory responses do not need to be as large or frequent.
When socially isolated, this relationship reverses. There is no need for a robust immune system, as being alone means low likelihood of contracting spreadable diseases. However, being on our own makes us more predisposed to sustaining a life threatening injury. We must do all that we can to survive. Inflammation increases to help us survive any major wounds.
This phenomenon is called the Conserved Response to Adversity; a change in genetic expression from social isolation. This swing increases short term survival, yet has dire consequences if occurring long term.
The crazy part? You don’t need to be in a tribe at all times to get the benefits of a community. Merely feeling connected to others or feeling loneliness can cause this change in expression.

Loneliness is when one’s needs are not being met by quantity or quality of social relationships. Feeling loneliness has been shown to predict depressive symptoms, worsen sleep, reduce physical activity, contribute to cognitive decline, increase blood pressure, set off the HPA axis, cause inflammation, reduce immune activity, and increase aging.
There are many ways to help improve loneliness feelings—cognitive behavioral therapy, meditation, and yoga—but perhaps the most important and effective is finding purpose. If you have purpose, loneliness can melt away!
Sum Up
A wide range of topics were covered by Bryan in one of the most comprehensive, physiology-based seminars I have ever had the pleasure of attending. If you get a chance, learning from this man is a must!
To summarize:
- Blood chemistry is a useful method for exploring multiple physiological processes.
- Glucose, both fasting and postprandial, must stay in a tight range for cells to stay healthy.
- High LDL and normal HDL are desirable markers to have for fat metabolism.
- Oxygen is essential for cellular metabolism, and can be measured by hemoglobin.
- Infections occur more often than we think, and specific pathologies can be elucidated with a complete blood count.
- ESR and CRP are effective inflammation markers
- Looking at bile acids and fatty liver index are better predictors of liver dysfunction than classic measurements, including biopsy.
- We are exposed to many environmental chemicals; supporting fat loss and detoxification can help with xenobiotic removal.
- Perceived social isolation has several negative health effects, but can be overcome by purpose.
What has been your experience with functional medicine? Comment below and let the fam know!
Cover photo by Gerd Altmann from Pixabay