Tag: exercise
Course Notes: Postural Respiration
Another Course in the Books As an official Ron Hruska groupie, the tour continued to the Big Apple to learn…
The Post Wonderful Time of the Year: Top Posts of 2013
The Best…Around Time is fun when you are having flies. It seems like just yesterday that I started up this…
Treatment of Shredded Cheese of the Hip: A Case Report and Rant
A Long Day I officially eclipsed my longest work day ever. Started seeing patients at 7:30 am and finished training…
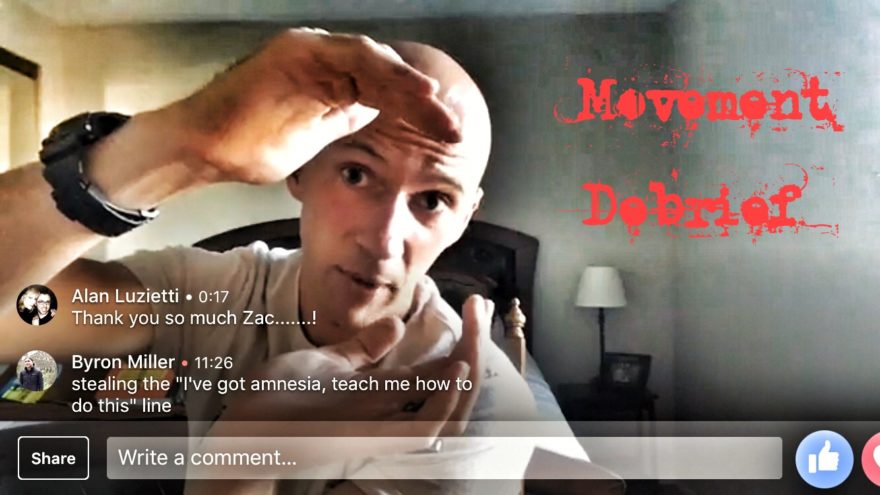
Chapter 14: Advanced Corrective Strategies
This is a chapter 14 summary of the book “Movement” by Gray Cook. Inputs Corrective exercise is focused on…
Movement Chapter 13: Movement Pattern Corrections
This is a chapter 13 summary of the book “Movement” by Gray Cook. Back to the Basics Mobility deficits…
Movement Chapter 12: Building the Corrective Framework
This is a chapter 12 summary of the book “Movement” by Gray Cook. A Whole Lotta P When we…
Movement Chapter 11: Developing Corrective Strategies
This is a chapter 11 summary of the book “Movement” by Gray Cook. Autonomics All exercise affects tone and tension.…
Movement Chapter 10: Understanding Corrective Strategies
This is a chapter 10 summary of the book “Movement” by Gray Cook. Mistakes, I’ve Made a Few When we…