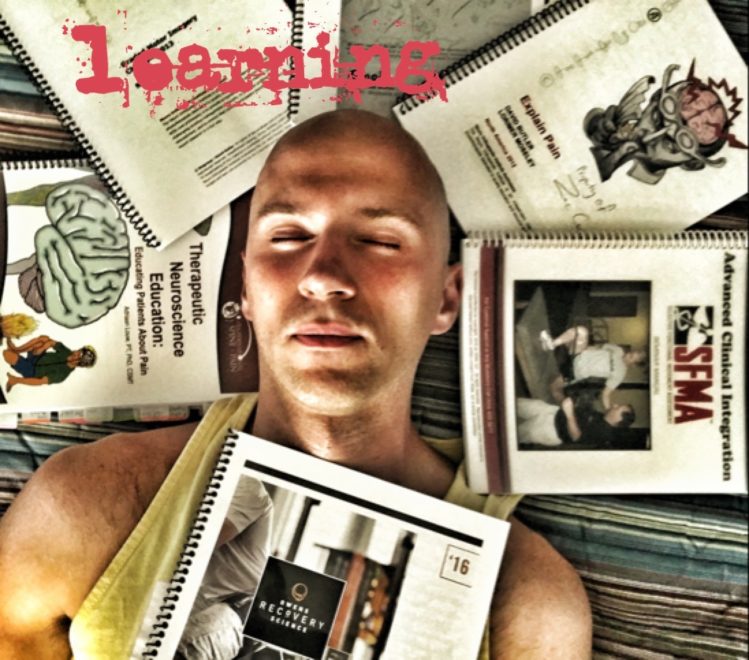
75 That’s my number. No, not that number. 75 is the number of continuing education classes, conferences, home studies, etc that I’ve completed since physical therapy school. Though the courses are many, it was probably too much in a short period of time. When quantity is pursued, quality suffers. Sadly, I didn’t figure out how to get the most out of each class until the latter end of my career. Two classes in particular stand out: Mobilisation of the Nervous System by the NOI Group, and ART lower extremity. Yes, the content was great, but these classes stood out for a different reason. You see, instead of just doing a little bit of prep work, I kicked it up a notch. I extensively reviewed supportive material, took impeccable notes, and hit all the other essentials needed to effectively learn. I was prepared, and because I was prepared I got so much more out of these classes than my typical fair. The lessons learned in those courses stick with me to this day. For the stuff you really want to learn, I’ll encourage you to do the same. Here is the way to get the most out of your continuing education. By the time you are done reading this post, you’ll understand why I now recommend a more focused learning approach and fewer courses. Let’s see how to do it.
Read More