Tag: education
Asymmetries, Foot Position, and Educating Practitioners – Movement Debrief Episode 105
Movement Debrief Episode 105 is in the books. Below is a copy of the video for your viewing pleasure, and…
Rib Rotation, Shoulder Issues, and Biomedical Education – Movement Debrief Episode 98
Movement Debrief Episode 98 is in the books. Below is a copy of the video for your viewing pleasure, and…
Shoes, Self-Correction, and Position Education – Movement Debrief Episode 95
Movement Debrief Episode 95 is in the books. Below is a copy of the video for your viewing pleasure, and…
Zone of Apposition, Total Hip Replacement, and Client Wants vs Needs – Movement Debrief Episode 74
Movement Debrief Episode 74 is in the books. Below is a copy of the video for your viewing pleasure, and…
Sitting Posture, Hypermobility, and Fear-Avoidance – Movement Debrief Episode 72
Movement Debrief Episode 72 is in the books. Below is a copy of the video for your viewing pleasure, and…
Exercise Dosing, Crossfit Shoulder Injuries, Regional Interdependence Education – Movement Debrief Episode 57
Movement Debrief Episode 57 is in the books. Below is a copy of the video for your viewing pleasure, and…

How to Communicate with People in Pain
Communicating with people in pain is a tricky situation. If you say the wrong thing, or act afraid amidst pain,…
Neck Strength, Narrow Infrasternal Angles, and My Joint Went Out! – Movement Debrief Episode 46
Movement Debrief Episode 46 is in the books. Below is a copy of the video for your viewing pleasure, and…

D League Readiness Measures, Navigating Flare-ups, and Should I get the OCS? – Movement Debrief Episode 16
Just in case you missed last night’s Movement Debrief Episode 16, here is a copy of the video and audio…

How to Design a Comprehensive Rehab Program
Just when I thought I was out, the clinic pulls me back in. Though I’m glad to be back. There’s…
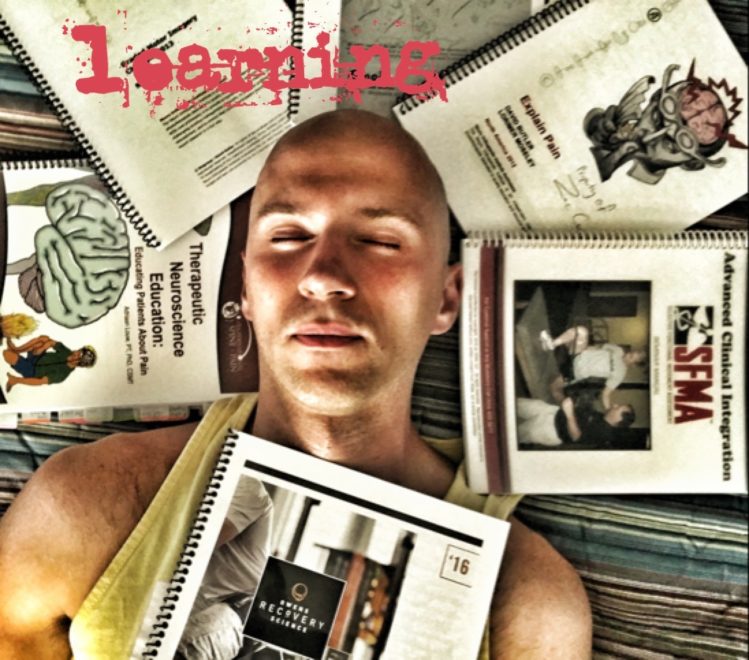
Continuing Education: The Complete Guide to Mastery
75 That’s my number. No, not that number. 75 is the number of continuing education classes, conferences, home studies,…
The 6-Step Method to Reading the Shit Out of Books
What Were We Talking About Again? If there is one thing I’ve struggled with over the years, it’s long-term retention.…
Explain Pain Section 6: Management Essentials
This is a summary of section 6 of “Explain Pain” by David Butler and Lorimer Moseley. Management 101 The most…

