Tag: therapeutic neuroscience education
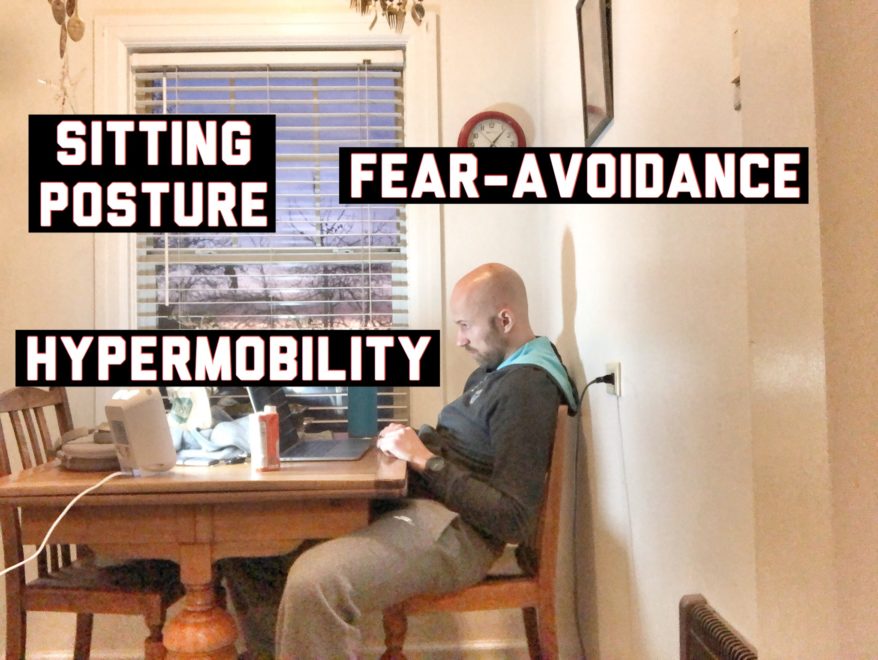
Sitting Posture, Hypermobility, and Fear-Avoidance – Movement Debrief Episode 72
Movement Debrief Episode 72 is in the books. Below is a copy of the video for your viewing pleasure, and…

How to Design a Comprehensive Rehab Program
Just when I thought I was out, the clinic pulls me back in. Though I’m glad to be back. There’s…
Come Hang With Me: Courses At My Clinic
Dear Readership We are hosting several courses at my clinic this year, and we would love to have you, the…
The Post Wonderful Time of the Year: 2014 Edition
And That’s a Wrap It’s that time of the year that we get to look back and reflect and what…
Pain Language and other Jive Talk
To All My Clinicians in the Struggle I struggle with patients. Those patients that I am having trouble with are…
PRI and Pain Science: Yes You Can Do It
Questions You may have noticed that my blogging frequency has been a little slower than the usual, and I would…


